Request a demo specialized to your need.
A standards-aligned playbook that turns PV signals into clear, explainable benefit–risk decisions.
Why the Signal Is No Longer the Problem
For most of my career in pharmacovigilance, the industry has treated signal detection as the pinnacle of safety science. If you could detect signals early, quantify them statistically, and escalate them through governance, you were doing your job well. And for a long time, that framing made sense. Signals were scarce, data was fragmented, and the risk of missing a signal was far greater than the risk of misinterpreting one.
That world no longer exists.
Today, pharmacovigilance teams are drowning in signals—from spontaneous reports, EHRs, registries, social media, literature, companion diagnostics, wearables, and real-world evidence (RWE). The challenge is no longer finding signals. The challenge is deciding which signals matter, why they matter, and how they change the product’s benefit–risk profile in a defensible, regulator-ready way.
This is where many PV organizations are failing.
Signals are detected, logged, triaged, and archived—but they do not reliably translate into coherent benefit–risk decisions. Instead, we see fragmented assessments, reactive regulatory responses, and benefit–risk narratives that are reconstructed under inspection pressure rather than continuously built over time.
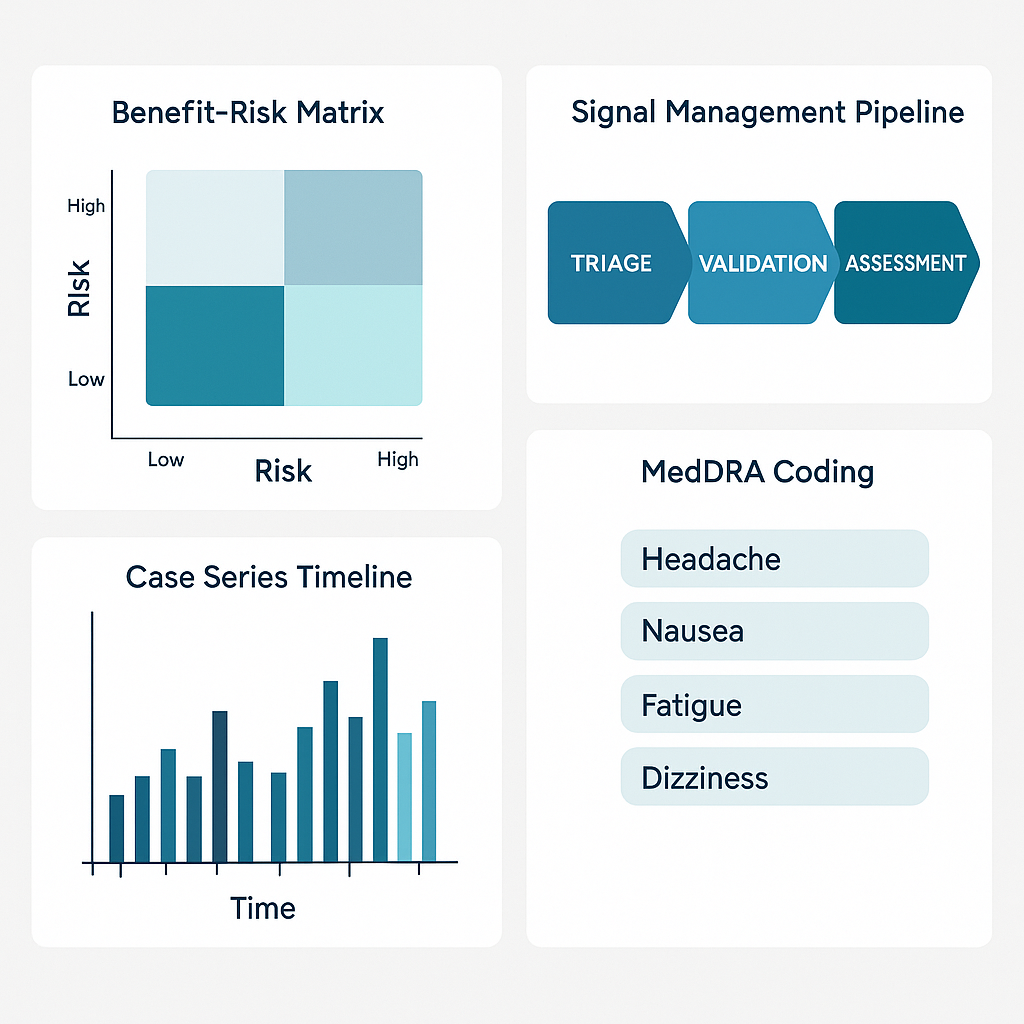
This article presents a modern PV playbook—one that moves deliberately from signal → insight → decision → benefit–risk, and treats benefit–risk not as a document, but as a living system of evidence, judgment, and accountability.
Part 1: The Structural Failure of Traditional Signal Management
1. Signal Detection Has Become a Commodity
Disproportionality analysis, Bayesian methods, observed-to-expected ratios, and data mining algorithms are now table stakes. Most global safety databases can produce statistically significant signals on demand. AI and machine learning have further accelerated this capability.
Yet despite this sophistication, regulatory findings related to inadequate signal evaluation and benefit–risk justification continue to rise.
Why?
Because signal detection answers the wrong question.
Detection asks:
“Is something unusual happening?”
But benefit–risk asks:
“Does this change what we believe about the product’s overall value to patients?”
The industry has invested heavily in the first question and underinvested in the second.
2. Signals Are Still Managed in Isolation
In many organizations, signals live in operational silos:
-
Signal detection systems
-
Aggregate reporting tools
-
Risk management plan (RMP) documents
-
Clinical development data repositories
-
Regulatory correspondence archives
Each system has its own workflows, owners, and governance. As a result:
-
Signals are evaluated without full clinical context
-
Benefit data is static or outdated
-
Risk minimization effectiveness is rarely measured
-
Decisions are documented, but not traceable
The consequence is a linear, document-driven process in a world that demands continuous, evidence-driven reasoning.
3. Benefit–Risk Is Still Treated as a Periodic Exercise
Most benefit–risk assessments are triggered by events:
-
Periodic reports (PSUR/PBRER)
-
Label changes
-
Regulatory questions
-
Major safety signals
This episodic approach assumes that benefit–risk is stable between reporting cycles. In reality, benefit–risk evolves continuously, shaped by:
-
New indications
-
Off-label use
-
Population shifts
-
Long-term exposure
-
Real-world outcomes
When benefit–risk is treated as a snapshot instead of a timeline, organizations are perpetually reacting to regulators instead of leading the narrative.
Part 2: Reframing Signal Management as a Decision System
The fundamental shift required in modern PV is this:
Signals are not outputs. They are inputs into a decision system.
A signal only has value if it contributes to:
-
A change in understanding
-
A change in behavior
-
A change in benefit–risk posture
This requires a new playbook built around four connected layers.
Layer 1: Signal Intelligence (Beyond Detection)
What Must Change
Traditional signal management focuses on statistical significance. Modern signal intelligence focuses on decision relevance.
Key questions shift from:
-
“Is this statistically significant?”
to: -
“Is this clinically meaningful?”
-
“Is it biologically plausible?”
-
“Is it preventable, predictable, or manageable?”
-
“Does it affect benefit in a specific population?”
What Leading PV Teams Do Differently
-
Combine quantitative signals with clinical phenotype analysis
-
Contextualize signals against exposure, indication, and disease severity
-
Classify signals by decision impact, not just seriousness
-
Track signal evolution over time, not as one-off events
The goal is not fewer signals—but fewer irrelevant escalations.
Layer 2: Integrated Evidence Assembly
Why Evidence Fragmentation Is the Silent Killer
Most signal assessments fail not because data is missing, but because data is disconnected.
Benefit–risk decisions require simultaneous visibility into:
-
Safety data (ICSRs, trends, severity)
-
Clinical efficacy endpoints
-
Real-world effectiveness
-
Patient-reported outcomes
-
Risk minimization measures
-
Regulatory commitments
When these elements live in different systems, PV teams are forced to manually reconstruct the story every time scrutiny arises.
The Modern Standard
Leading organizations are moving toward continuous evidence assembly, where:
-
Signals automatically pull relevant benefit context
-
Prior decisions and rationales are linked
-
Assumptions are explicit and auditable
-
Evidence gaps are visible, not hidden
This transforms signal evaluation from an opinion exercise into an evidence-backed judgment process.
Layer 3: Decision-Centric Governance
The Myth of the Safety Committee
Most safety governance bodies are structured around review, not decision. They receive summaries, debate interpretations, and approve actions—but often without:
-
Clear decision criteria
-
Explicit risk tolerance thresholds
-
Defined escalation triggers
As a result, similar signals may receive different outcomes, depending on timing, personalities, or regulatory pressure.
A Better Model: Decision Playbooks
Modern PV organizations define:
-
What decisions can be made at which signal confidence levels
-
What evidence is required for each decision type
-
When benefit–risk must be formally re-evaluated
-
How uncertainty is documented and revisited
This creates consistency without rigidity—and defensibility without bureaucracy.
Layer 4: Living Benefit–Risk Narratives
Benefit–Risk Is Not a Document
A benefit–risk assessment should never be a static PDF assembled weeks before submission. It should be a living narrative that evolves as evidence evolves.
In high-performing organizations:
-
Every major signal updates the benefit–risk storyline
-
Rationale for “no action” decisions is explicitly recorded
-
Risk minimization effectiveness feeds back into benefit–risk
-
Regulatory questions can be answered from existing traceability
This shifts PV from compliance-driven reporting to proactive regulatory storytelling.
Part 3: The Contrarian View — Why “Early Signal Detection” Is Overrated
One of the most widely accepted best practices in PV is:
“The earlier you detect a signal, the better.”
This is only partially true.
Early detection without decision readiness often leads to:
-
Premature escalations
-
Over-labeling
-
Inconsistent global actions
-
Erosion of benefit narratives
In reality, regulators are not asking:
“Did you detect the signal early?”
They are asking:
“Did you understand it correctly, act proportionately, and protect patients without undermining benefit?”
A late but well-reasoned, evidence-based decision is often more defensible than an early but poorly contextualized one.
The future of PV excellence lies not in speed alone—but in judgment quality.
Part 4: The PV Playbook — From Signal to Benefit–Risk
Step 1: Classify Signals by Decision Impact
Not all signals deserve the same attention. Classify them by:
-
Potential to alter benefit–risk
-
Population specificity
-
Preventability
-
Regulatory sensitivity
Step 2: Assemble Evidence Automatically
For each priority signal, assemble:
-
Safety trends
-
Benefit endpoints
-
Exposure context
-
Prior regulatory positions
-
Existing risk controls
Step 3: Make the Decision Explicit
Document:
-
What decision was made
-
Why alternative actions were rejected
-
What uncertainty remains
-
When reassessment will occur
Step 4: Update the Benefit–Risk Narrative
Continuously update:
-
Key risks and benefits
-
Risk mitigation effectiveness
-
Population-specific considerations
Step 5: Close the Loop
Feed outcomes back into:
-
Signal thresholds
-
Risk management strategies
-
Development and labeling decisions
Conclusion: From Compliance to Confidence
Pharmacovigilance is at an inflection point.
The organizations that succeed in the next decade will not be those with the most signals, the fastest algorithms, or the largest databases. They will be the ones that can confidently explain, at any moment, why their product’s benefits continue to outweigh its risks—and what they are doing about the uncertainty that remains.
That confidence is not built at submission time.
It is built every day—from signal to benefit–risk.
And that is the new PV mandate.
Subscribe to our Newsletter

